Here, we are sharing information on the topic of “cervical cancer means.” Cancer of the cervical cells is known as cervical cancer. The most crucial actions you can take to avoid cervical cancer are to have regular gynecological checkups, have Pap tests, and engage in safe sexual behavior. The three basic therapies for cervical cancer are surgery, radiation therapy, and chemotherapy.

cervical cancer means
Cervical cancer: What is it?
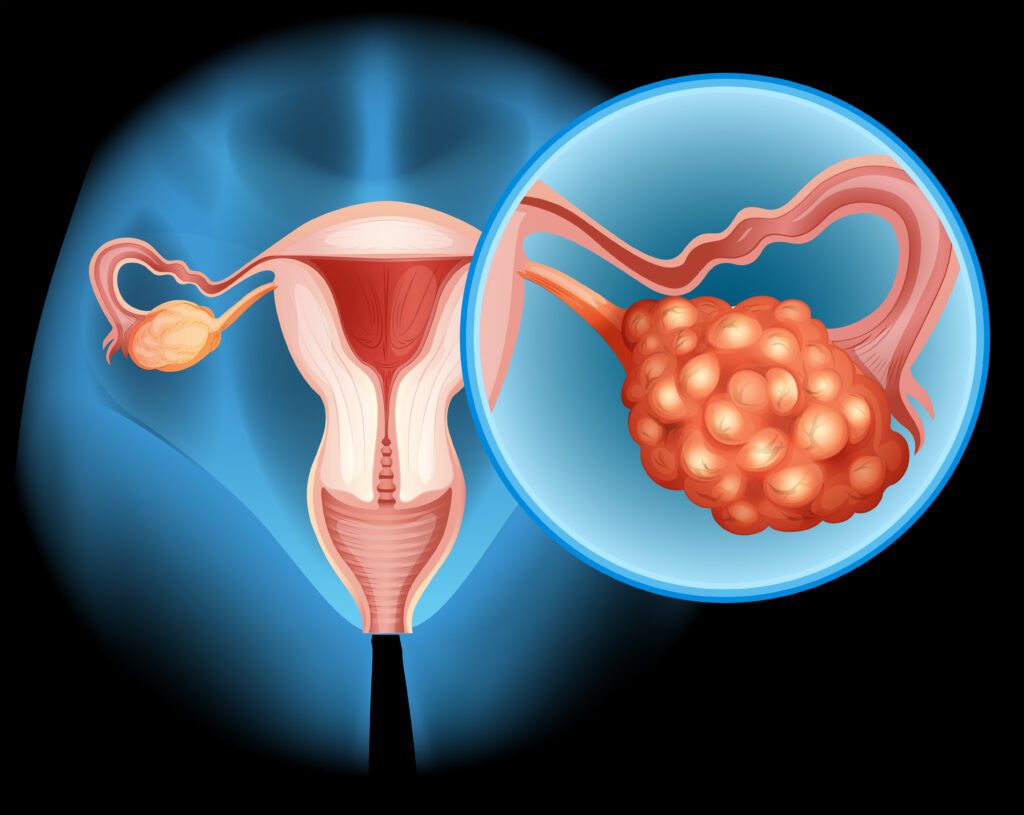
Your cervix’s surface is where cervical cancer, also known as cancer of the cervix, first appears. It occurs when precancerous cells start to emerge from the cells on your cervix. Cervical cancer can be prevented by identifying precancerous cells and treating them before they transform, even though not all of these cells will eventually become cancerous.
Cervical cancer types
Cervical cancers primarily manifest as adenocarcinomas or squamous cell carcinomas. Squamous cell carcinomas account for about 80% to 90% of cervical cancer cases, while adenocarcinomas make up 10% to 20%.
What is the cervical region?
The lowest point of your uterus is called the cervix (where a baby grows during pregnancy). It joins the opening of your vagina to your uterus and has a somewhat donut-like appearance. Tissues consisting of individual cells cover it. These are the cells that are healthy enough to develop into precancerous cells.
What is the prevalence of cervical cancer?
Every year, over 14,000 Americans receive a cervical cancer diagnosis. The most common age range for cervical cancer diagnoses is 35 to 44 years old. 50 is the typical age at diagnosis. Every year, almost 4,000 people pass away from cervical cancer. The HPV vaccine and screenings have led to a decrease in this rate.
Signs and symptoms of cervical cancer
Seldom do precancerous alterations in cervical cells result in symptoms. Cervical screening is the only technique to determine whether aberrant cells have the potential to develop into cancer. The following are the most typical indicators that cervical cancer may arise from early cell changes:
- vaginal bleeding in between menstruations
- thicker or longer-lasting menstrual flow than normal
- discomfort during sexual activity
- bleeding following a sexual encounter
- pelvic discomfort
- a change in your vaginal discharge, such as an increase in volume or the presence of an intense or peculiar color or odor
- bleeding from the vagina after menopause.
Other disorders may be the cause of these symptoms, but if you are concerned or the symptoms don’t go away, see your doctor.
cervical cancer causes
- The largest risk factor for cervical cancer is chronic infection with certain high-risk strains of the human papillomavirus (HPV), which accounts for almost all occurrences of the disease. Smoking is the other major risk factor for cervical cancer.
- There is some evidence that women who have used the pill for birth control for five years or longer are more likely to get HPV-related cervical cancer. It has been demonstrated that using the pill lowers the risk of developing ovarian and uterine malignancies, while the risk is still minimal.
Additional risk variables consist of the following:
- both active and passive smoking
- A compromised immune system
If your mother was given the prenatal medication diethylstilbestrol (DES), which is a synthetic version of the female hormone estrogen (between 1939 and 1971),
Eight out of ten women will, at some point in their lives, contract genital HPV. Cervical cancer is an uncommon outcome of HPV infection; the majority of women who have the virus never develop cervical cancer.
The detection of cervical cancer
You will be referred to a specialist for additional testing if the results of your screening test indicate that you may be experiencing cancer symptoms.
Tests commonly used to identify cervical cancer include:
A biopsy combined with a colposcopy
- The location and appearance of abnormal cells in the cervix are determined via a colposcopy. A speculum is put into your vagina so the physician can use a colposcope—a device that magnifies the area—to inspect your cervix and vagina.
- It is not inserted into your body; rather, it is placed next to your vulva. A colposcopist, typically a gynecologist or, in certain clinics, a nurse practitioner, performs the procedure.
Cervical cancer treatment and staging
In the event that cervical cancer is discovered, it will be graded, going from stage 1, which indicates that abnormal cells are only present in the cervix’s tissue, to stage 4, which indicates that the disease has progressed to the lung, liver, or bones in addition to the pelvis. This aids in the care your doctors are planning for you.
Treatment modalities
- The stage of the disease determines the course of treatment. Surgery is the first line of treatment for early, non-bulky illness (less than 4 cm), with chemoradiation therapy sometimes used in addition.
- A cone biopsy might be enough if the tumor is tiny; in other situations, a hysterectomy—the surgical removal of the uterus—may be necessary.
- A combination of chemotherapy (cisplatin) and radiation therapy (radiation therapy) is utilized for locally advanced illness.
- Treatment options for metastatic illness include palliative care alone or chemotherapy (platinum or fluorouracil).
Cervical cancer screening
The cervical screening test has replaced the pap smear.
Since the National Cervical Screening Program was implemented in 1991, Australia has seen a halving of the incidence and mortality rates associated with cervical cancer. Women between the ages of 18 and 70 could receive a free Pap smear screening every two years through this program.
The cervical Screening Test has taken the place of the Pap smear as of December 1, 2017. The majority of women in the programme, who are 25 to 74, will be examined every five years. Your first HPV test should be scheduled two years following your most recent Pap smear test if you have already had one.
Predictability of cervical cancer
- The precise course of an illness cannot be predicted by a doctor because it depends on the unique circumstances of each patient. However, depending on the type of cervical cancer you have, test results, tumor growth rate, age, level of fitness, and medical history, your doctor may provide you with a prognosis, or the expected course of the disease.
- When detected early, cervical cancer can be efficiently treated. The majority of women who have cervical cancer early on will recover.
- Getting pregnant could become more challenging or impossible after receiving treatment for cervical cancer. Prior to starting therapy, discuss with your doctor any concerns you may have about conception.
Frequently asked question
(cervical cancer means)
Can cervical cancer be cured?
Answer: A radical hysterectomy procedure is used to treat the majority of cervical malignancies that have not progressed outside the cervix. This entails the excision of the uterus, cervix, vaginal wall, and adjacent lymph nodes. Frequently, a hysterectomy will both cure the cancer and prevent it from returning.
What happens after cervical cancer?
Answer: Following a radical hysterectomy, the majority of women will also require 8 to 12 weeks out from work to recuperate. Chemotherapy and radiation are two therapies for cervical cancer that can cause extreme fatigue. You might need to temporarily pause some of your regular activities as a result.
Is cervical cancer painful?
Answer: Signs and Symptoms of Cervical Cancer | Moffitt
Sometimes, a dull backache or hazy feelings of pressure or weight in the pelvis can be symptoms of cervical cancer. On the other hand, pain from an early-stage tumor could be negligible or even minimal.
Conclusion
(cervical cancer means)
The conclusion regarding cervical cancer:
A major global health concern, millions of women are impacted by cervical cancer every year. It is still the primary cause of cancer-related deaths among women, even with advances in prevention, identification, and treatment. This is especially true in underdeveloped nations where access to screening and medical care may be restricted.
Proactive steps like HPV vaccination and routine screenings have demonstrated potential in lowering the incidence and fatality rates of cervical cancer. Nonetheless, more access, education, and knowledge of these treatments are still required, particularly for marginalized communities.
So, this is how the topic “cervical cancer means” has been addressed.
- For more information related to these topics, click here.
- You may also visit our Instagram page by clicking here.
- You may also visit our YouTube channel by clicking here






